30 Common Skin Rash Pictures - How to ID Skin Rash Symptoms
How Is Bacterial Vaginosis Different From A Yeast Infection?
Bacterial vaginosis (BV) and vaginal yeast infections can both cause pain and discomfort, difficulty urinating, and itching. Other symptoms, such as vaginal discharge, may differ. Treatment will depend on which infection a person has.
A yeast infection and BV are both infections that cause vaginitis.
Vaginitis is the medical term for inflammation of the vagina. It can lead to uncomfortable symptoms, including:
Below, we describe the differences between BV and a yeast infection. In particular, we explore the symptoms of both issues and the steps a person can take to prevent them.
BV and yeast infections have different causes and risk factors, but both cause inflammation of the vagina — vaginitis. In fact, these infections are two of the most common causes of vaginitis.
When a doctor diagnoses a cause of vaginitis, the cause is:
It can sometimes be hard to tell whether a person has BV or a yeast infection, but there are some characteristic signs.
The table below summarizes similarities and differences in the symptoms of BV and a yeast infection:
BV causes"Vaginal flora" collectively refers to the bacteria that live in the vagina.
Usually, among the vaginal flora, there is more of a type of helpful bacteria, called Lactobacillus, than harmful bacteria.
Certain activities can disrupt the natural balance of the microorganisms in the vagina, and this disruption leads to BV.
Risk factors for BV include:
Bacteria do not cause vaginal yeast infections. Instead, the cause is usually a type of fungus, or yeast, called Candida.
This fungus can be naturally present in the vaginal area, but Lactobacillus bacteria usually restrict the growth of Candida.
However, in some situations, Candida multiplies unchecked, leading to a yeast infection.
Risk factors for a yeast infection include:
To determine whether a vaginal infection is BV or a yeast infection, a doctor may:
Around 20% of healthy females tend to have Candida in their vaginas, so a positive fungal culture does not necessarily indicate that the fungus is responsible for any symptoms.
The treatments for BV and a yeast infection are different. Also, the right course of treatment can depend on the severity of the infection.
BV treatmentTo treat BV, a doctor may prescribe antibiotic medications, such as:
If a person experiences mild to moderate symptoms of a yeast infection, a doctor may recommend one of the following antifungal medications:
If a person has a severe yeast infection, a doctor may recommend taking a long course of antifungal medication, involving multiple doses.
Some strains of Candida are resistant to conventional medications. When one of these strains is causing the infection, the doctor will recommend special antifungal treatments.
It is not always possible to prevent BV or a yeast infection. However, doing the following can reduce the risk:
BV and a yeast infection can cause similar symptoms, though there are telltale differences.
Different issues cause the two infections, so they require different treatments.
BV results from an overgrowth of harmful bacteria in the vagina, while an overgrowth of Candida fungus causes a yeast infection.
Both infections cause changes in vaginal discharge. BV causes thin discharge with a fishy odor, while a yeast infection causes discharge that is thick and odorless.
Doctors typically recommend antibiotic medications to treat BV and antifungal medications to treat yeast infections. Also, over-the-counter tablets, creams, ointments, and suppositories are available to treat mild to moderate yeast infections.
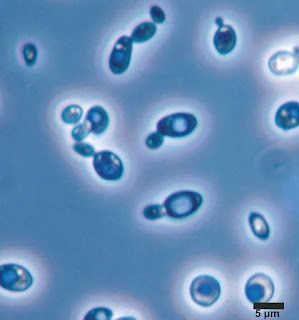
Fission Yeast Schizosaccharomyces Pombe And Budding Yeast Saccharomyces Cerevisiae Cells Under Microscope
Fission yeast Schizosaccharomyces pombe and budding yeast Saccharomyces cerevisiae cells under microscope
Fission yeast and budding yeast are free-living haploid cells that are easily grown in the laboratory. They have different cell shapes and patterns of division. Left, fission yeast; right, budding yeast; visualized with the nuclear DNA stain DAPI (4',6-diamidino-2-phenylindole) to highlight the nucleus.
Different models of cell cycle regulation converged when scientists realized that different model organisms shared the same molecules. See how data from frogs and yeast were reconciled.
What Is A Bladder Infection?
A bladder infection is a type of UTI, which refers to infection in the bladder, kidneys, ureters, or urethra.
A bladder infection is most often caused by a bacterial infection within the bladder. For people with weakened immune systems, yeast can cause bladder infections as well.
Bacterial infections can cause the bladder to inflame, which is a condition known as cystitis.
Most cases of bladder infections are acute, meaning they occur suddenly. Other cases may be chronic, meaning they recur over the long term. Early treatment is key to preventing the spread of the infection.
A bladder infection is a type of urinary tract infection (UTI). This refers to an infection anywhere in the urinary tract, such as the:
The upper urinary tract includes the kidneys and ureters. The kidneys filter blood to remove waste, producing urine. The ureters carry the urine to the lower tract.
The lower tract includes the bladder and urethra. Your bladder acts as a reservoir, storing urine until you're ready to release it. Urine is passed out of the body through the urethra.
UTIs occur more often in the lower tract as it's easier for bacteria to enter.
Bacteria that enter through the urethra and move into the bladder can cause infections. Typically, the body removes the bacteria by flushing them out during urination.
Bacteria can sometimes attach to the walls of your bladder and multiply quickly. This overwhelms the body's ability to destroy them, resulting in a bladder infection.
Most bladder infections are caused by Escherichia coli (E. Coli). This type of bacteria is naturally present in the large intestines.
An infection can occur when bacteria from your stool get on your skin and enter your urethra. In women, the urethra is short and the outside opening is not far from the anus, so bacteria can easily move from one body system to another.
The symptoms of a bladder infection vary depending on the severity. You'll immediately notice changes during urination. Some of the most common symptoms include:
When bladder infections spread, they can also cause mid-back pain. This pain is associated with an infection in the kidneys. Unlike muscular back pain, this pain will be persistent regardless of your position or activity.
A kidney infection will often cause:
You'll typically feel quite ill. Kidney infections are more serious than bladder infections and require urgent medical attention.
Anyone can get bladder infections, but there are different risks for women and men.
Bladder infections in womenWomen are more prone to getting bladder infections than men. About 40 percent of women in the United States develop a urinary tract infection at some point in their life.
This is because women have shorter urethras, making the path to the bladder easier for bacteria to reach. Women's urethras are also located closer to the rectum than men's urethras. This means there is a shorter distance for bacteria to travel.
During pregnancy, changes in the urinary tract increase the risk of an infection. Changes in the immune system also increase risk during pregnancy.
Some forms of birth control, like diaphragms and spermicides, may increase your risk of urinary tract infections.
Women are also more prone to recurring infections. About 25 percent of women will experience a second infection within 6 months of their first infection.
Bladder infections in menAs men age, the prostate can enlarge. This can cause blockages to the flow of urine and increase the likelihood of developing a UTI. UTIs tend to increase in men as they age.
Bladder infections are not very common in men less than 65 years old. However, younger men who are uncircumcised or have anal sex may be at greater risk.
Other risk factorsOther factors can increase the risk of bladder infections for both men and women. These include:
A doctor can diagnose your bladder infection by performing a urinalysis. This is a test performed on a sample of urine to check for the presence of:
Your doctor may also perform a urine culture, which is a test to determine the type of bacteria in the urine causing the infection.
Once they know the type of bacteria, they will test it for antibiotic sensitivity to determine which antibiotic will best treat the infection.
You can connect with a primary care doctor or a urologist in your area using the Healthline FindCare tool.
Bladder infections are treated with prescription medications to kill the bacteria, usually antibiotics, and medications that relieve pain and burning.
MedicationOral antibiotics are used to kill the bacteria that are causing the bladder infection.
If you're experiencing pain and burning sensations, your doctor may also prescribe medication to relieve those symptoms.
The most common medication for relieving the pain and burning associated with bladder infections is called phenazopyridine (Pyridium).
Home treatmentIn addition to antibiotics, there are steps you can take at home to help treat your bladder infection:
Certain lifestyle changes may reduce your chances of getting a bladder infection.
If you've been experiencing recurrent bladder infections, your doctor may recommend prophylactic treatment. This consists of antibiotics taken in small daily doses to prevent or manage future bladder infections.
Lifestyle changesSome of the following lifestyle changes may help reduce or eliminate the occurrence of bladder infections:
If you're experiencing recurrent bladder infections, your doctor may give you a prescription for daily antibiotics to prevent infections or to take when you feel the symptoms of a bladder infection.
They may also have you take a single dose of an antibiotic after sexual activity.
Most bladder infections subside within 48 hours of taking the appropriate antibiotic. It's important to finish all antibiotics prescribed, even if you're feeling better.
Some bladder infections can worsen and spread to the kidneys due to antibiotic-resistant strains of bacteria, delayed or inadequate treatment, or other health issues.
If you have recurrent UTIs, it's important to contact your doctor. You may need certain tests to make sure your urinary system is otherwise healthy.
If you don't already have a primary care physician, you can browse doctors in your area through the Healthline FindCare tool.
Chronic bladder infections require a combination of treatment and preventive measures. Long-term daily antibiotics may be necessary in some cases.
Being proactive about bladder infections can help reduce their occurrence as well as the pain and possible complications that accompany them.
The earlier you seek treatment, the less likely it is that the infection will spread, and the sooner you'll feel better.

Comments
Post a Comment