Robert Zakar gives back to community
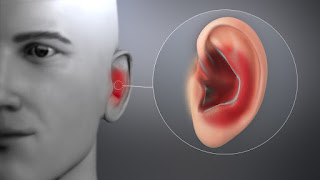
Ear Infections Causes, Symptoms, And Treatment
Experiencing inner ear discomfort or constant pressure, pus drainage, or hearing loss may be symptoms of an ear infection. You can use over-the-counter (OTC) treatments or consult a doctor if your symptoms don't improve.
Ear infections can be either bacterial or viral infections. They can occur in your middle ear, the part of your ear just behind your eardrum, as well as the outer and inner ear. They often clear up on their own but can be painful due to inflammation or fluid buildup.
Ear infections can be chronic or acute. Acute ear infections are painful but short in duration. Chronic ear infections either don't clear up or recur many times. They can cause damage to the middle and inner ear, which is infrequently permanent.
Keep reading to learn about ear infections, including causes, symptoms, and treatment options.
Common symptoms of ear infections include:
These symptoms might persist or come and go. Symptoms may occur in one or both ears. Pain is usually more severe with a double ear infection, which is an infection in both ears.
Chronic ear infection symptoms may be less noticeable than those of acute ear infections.
Symptoms of an ear infection in childrenAlong with symptoms seen in adults, such as ear pain and drainage, young children and babies may show other signs of an ear infection, such as:
Usually, ear infections last fewer than 3 days, but they can persist for up to a week.
Children younger than 6 months who have a fever or other ear infection symptoms should see a doctor. Seek medical attention if your child has a fever higher than 102°F (39°C) or severe ear pain.
Ear infections are caused by viruses or bacteria, particularly the bacteria Streptococcus pneumoniaeor Haemophilus influenzae. They often result from a blockage of your Eustachian tubes, which causes fluid to build up in your middle ear. Eustachian tubes are small tubes that run from each of your ears directly to the back of your throat.
Causes of Eustachian tube blockage include:
Ear infections can also develop from infected adenoids. Your adenoids are glands on the roof of your mouth behind your nose that help protect your body from infections. Infections can spread from these glands to the nearby ends of your Eustachian tubes.
Risk factors for ear infectionsEar infections occur most commonly in young children because they have short and narrow Eustachian tubes. About 80 percent of children develop an acute ear infection at some point.
Infants who are bottle-fed also have a higher incidence of ear infections than their breastfed counterparts.
Other factors that increase the risk of developing an ear infection are:
Ear infections usually clear up without intervention, but they may recur. These rare but serious complications may follow an ear infection:
While most mild ear infections clear up without intervention, the following treatments can also help:
Home treatmentThese methods are effective in relieving the symptoms of a mild ear infection:
Medical treatmentIf your symptoms get worse or don't improve, see a doctor. They may prescribe antibiotics if your ear infection is bacterial, chronic, or doesn't appear to be improving.
Antibiotics don't help treat viral infections.
Medical treatment in childrenDoctors often take a wait-and-see approach when treating ear infections in children to avoid over-prescribing antibiotics, which can lead to antibiotic resistance.
A doctor may sometimes write you a prescription for antibiotics if symptoms are severe or don't resolve within 2 to 3 days. Alternatively, they may write you a prescription but recommend waiting first to see if your child's symptoms get better after 2 to 3 days.
It's important to finish your entire prescription. Often, a 7- or 10-day prescription of amoxicillin is prescribed.
You shouldn't give children aspirin without their doctor's instruction. Aspirin is a preventable risk factor for developing Reyes' syndrome, a rare disorder that causes brain and liver damage.
SurgerySurgery may be an option if your ear infection isn't eliminated with the usual medical treatments or if you have many ear infections over a short period.
Most often, ear tubes are placed in your ears to allow fluid to drain out. These tubes are surgically inserted into your eardrums. They eventually fall out and the holes heal over. Sometimes these holes need to be closed surgically.
A myringotomy surgery is another option. During this procedure, a doctor creates a small hole in your eardrum to let fluid drain and to relieve pain. The incision heals within a few days.
In cases that involve enlarged adenoids, surgical removal of your adenoids may be recommended.
The Centers for Disease Control and Prevention recommends seeing a doctor when your child has:
For adults, it's a good idea to visit a doctor if your symptoms last longer than 2 or 3 days, or you have severe pain or a fever.
A healthcare professional will consider your symptoms and examine your ears with an instrument called an otoscope that has a light and magnifying lens. The examination may reveal:
This exam is rarely painful, but some children may be bothered.
Additional testsOther tests include:
The following practices may reduce the risk of ear infection:
Ear infections are caused by bacteria or viruses in your middle ear, which is the part of your ear behind your eardrum. Most ear infections clear up within about 3 days, but severe infections may need to be treated with antibiotics.
Ear infections are most common in children. It's important to see a doctor if you or your child develop severe pain, a fever over 102.2°F, ear drainage, or other concerning symptoms.
Steps To Heal Otitis Externa (Swimmer's Ear)
Prescriptions ear drops are the mainstay of treatment
FangXiaNuo / Getty Images
Medically reviewed by John Carew, MD
Otitis externa, also known as swimmer's ear, is an infection of the outer ear canal that causes pain along with swelling, redness, itching, ear drainage, and decreased hearing.
Prescription ear drops are the mainstay of otitis externa treatment, some of which contain acidifying or drying agents. Bacterial and fungal otitis externa can be effectively treated with antibiotic or antifungal ear drops. Steroid ear drops can help ease itchiness and inflammation.
FangXiaNuo / Getty Images
This article explains how to heal swimmer's ear, including preferred treatment options and self-care tips. It also explains when it is time to see an ear, nose, and throat (ENT) specialist if complications arise that might permanently damage your hearing.
Related: Anatomy of the Ear: What You Should Know
Otitis Externa: A Common Outer Ear InfectionOtitis externa is a common ear infection that accounts for nearly 500,000 healthcare provider office or emergency room visits yearly. An estimated 10% of people will get otitis externa at some point in their life.
Otitis externa is called swimmer's ear because repeated exposure to water can make the ear canal vulnerable to inflammation. Inflammation, in turn, can disrupt the integrity of the skin in the ear and allow bacteria and fungus easier entry into underlying tissues.
This condition can affect all age groups. However, children who spend a lot of time in the water are at greatest risk, particularly during the summer months when swimming is common.
Symptoms of otitis externa often develop rapidly, usually within a span of 48 hours, and may include:
Ear pain (made worse by touching the ear canal, tugging the ear, or chewing)
Itchiness
Redness and swelling
A feeling of ear fullness
Swollen lymph nodes in the neck
Ear drainage with crusting
Muffled hearing
Fever
Jaw pain on the affected side
Otitis externa is most often caused by bacteria and less frequently by fungi. Swimming in contaminated water is a common way to get swimmer's ear. But you can also get it if water becomes trapped in the ear while showering or sweating, especially in humid climates.
Story continues
Other risk factors include:
Ear wax buildup
Having hairy ear canals
Using unclean hearing aids or earbuds
Wearing earplugs
Putting things into your ear (like cotton swabs or fingers)
Related: What It Means When Your Ear is Draining
Will Otitis Externa Heal Without Treatment?Unlike otitis media (middle-ear infection), which sometimes heals on its own, otitis externa generally won't go away without treatment. While milder cases may clear without medications, it can take weeks—and a lot of aggravation and discomfort—to get there.
Swimmer's ear is generally not serious, but a prolonged or severe infection can injure the ear canal and make it vulnerable to repeated infections (known as chronic otitis externa). Repeated infections, in turn, can cause the ear canal to narrow, potentially affecting hearing.
By treating otitis externa early with prescription ear drops, you can avoid complications and usually resolve the infection within a week or less.
When to Seek Otitis Externa TreatmentGiven the benefits of early treatment, it is important to see a healthcare provider if you even have mild symptoms of otitis externa. Early treatment almost invariably leads to better outcomes.
The diagnosis is relatively straightforward, and the treatment can readily be dispensed by a general practitioner. More complicated cases may require an ENT specialist known as an otolaryngologist.
The diagnosis of swimmer's ear involves a visual examination of the ear canal using a lighted scope called an otoscope. A swab of your ear canal may be cultured in the lab to determine if the cause is bacterial or fungal. This helps ensure that the correct treatment is dispensed.
A thorough diagnosis by a healthcare provider is important because otitis externa can mimic other conditions like eczema, psoriasis, and contact dermatitis that require different treatments.
Note to ParentsOtitis externa is not only common in children but also more likely to cause complications if left untreated. The spread of infection to the middle ear can lead to otitis media with effusion (OME), a potentially serious condition that can cause temporary or permanent hearing loss.
In infants and young children, even temporary hearing loss can lead to delays in speech development and social skills development.
Related: Common and Uncommon Causes of Ear Pain
Effective Otitis Externa TreatmentsPrescription ear drops are the mainstay of treatment for otitis externa. Oral painkillers are occasionally prescribed to help ease the pain.
The treatment may also involve the cleaning of the ear canal or the use of a tool called an ear wick to deliver medications into a blocked ear canal.
Types of Ear DropsDepending on the type and severity of infection involved, one or more ear drops may be prescribed. Each has a different mechanism of action that can either kill the underlying germ or make the environment of the ear hostile to the germ.
Ear drops commonly prescribed for swimmer's ear include:
Drying ear drops: Bacteria and fungi thrive in moist environments. These ear drops mainly contain isopropyl alcohol, which dries the ear canal and impedes the germ's growth.
Acidifying ear drops: These ear drops typically contain acetic acid, which is hostile to most bacteria and fungi. On the downside, the drops can cause stinging if tissues are inflamed.
Antibiotic ear drops: Ciprofloxacin ear drops are effective for bacterial infections. Ofloxacin, polymyxin B, and neomycin may also be used.
Antifungal ear drops: Clotrimazole, fluconazole, and miconazole ear drops may be prescribed to treat fungal ear infections.
Corticosteroid (steroid) ear drops: Hydrocortisone and dexamethasone can help ease inflammation and pain and are often the ingredients found in combination antibiotic ear drops.
Oral antibiotics taken by mouth are not used to treat otitis externa. On their own, they are insufficient to curb a bacterial infection and may only increase the risk of antibiotic resistance. The only exception is when the infection has spread outside of the ear canal.
Related: How to Use Ear Drops Correctly
Oral PainkillersEar pain is very rarely severe with otitis externa. Pain can make it difficult to sleep, work, or function. Oral painkillers, both over-the-counter and prescription, can often provide short-term relief.
Some of the more common options include:
Related: How to Manage Ear Pain Safely
Other ProceduresBefore ear drops can be used, the ear canal may need to be cleaned. This procedure, known as aural toileting, is performed by a healthcare provider (and never by yourself or a nonmedical professional).
The process usually involves:
Manually clearing the ear of any debris (like large pieces of wax)
Irrigating the ear canal with sterile fluids from a bulb syringe
Suctioning the ear canal with gentle vacuum pressure
If the ear canal cannot be adequately cleaned or is very swollen, a device called an otowick may be used. This spongy wick is inserted into the canal and expands when drops are applied, securing it in place. The wick can be left for several days, allowing the drops to travel deep into the ear canal when applied.
Related: Natural Remedies for Swimmer's Ear
Following Otitis Externa Antibiotic PrescriptionOtitis externa is more often than not caused by a bacterial infection and, with proper treatment, can heal within three to 10 days.
According to guidelines issued by the American Academy of Otolaryngology, the following antibiotic therapies can be used:
Ciprofloxacin with hydrocortisone: Three drops to the affected ear twice daily
Polymyxin B, neomycin, and hydrocortisone: Three to four drops to the affected ear four times daily
Ofloxacin: Five drops to the affected ear twice daily
The drops need to be administered without missing a dose. Be sure to space the doses as evenly as possible (every eight hours for ciprofloxacin, every six to eight hours for polymyxin B/neomycin, and roughly every five hours for ofloxacin).
The treatment can be extended up to 10 days, with up to 95% of people experiencing complete clearance within seven to 10 days.
How to Pay for TreatmentThe cost of treating any ear infection can often exceed $300. While insurance may cover some of the expenses, you may still be left with co-pay or coinsurance costs.
To reduce out-of-pocket costs, see if combination ear drops (which are generally more expensive) can be substituted with individual ear drops (which are generally less expensive).
You can also compare drug prices and get coupons on consumer websites like GoodRx or find low-cost drugs (like ofloxacin ear drops) from online retailers like Mark Cuban's CostPlus.
Self-Care With Otitis ExternaWhile undergoing treatment for otitis externa, there are five self-care tips that can ensure the best possible outcomes, which are:
Do not use any other ear drops unless your healthcare provider gives you the OK.
Avoid showering until the infection has cleared, instead opting for a bath. Make sure to keep the ear out of the bathwater.
If you have to shower, lightly coat a cotton ball with petroleum jelly to use as an earplug. Keep your ear away from the water stream. Do not use plastic earplugs.
After washing, use a hairdryer set on low to gently dry the ear.
To help ease the pain, place a warm, moist face cloth against the ear. You can do this several times a day for 10 to 15 minutes.
Otitis externa is considered acute if it lasts less than six weeks. If it lasts longer than three months, it is classified as chronic otitis externa.
Chronic otitis externa differs from acute otitis externa in that it is less likely to be caused by an infection and more likely to be caused by an allergy, autoimmune disease, or skin disease like psoriasis or eczema. These conditions often come and go in flares and can affect both ears rather than just one.
With chronic otitis externa, ear pain is uncommon. Instead, there may be itching (sometimes intense) along with muffled hearing in the affected ear. Over time, the persistent inflammation can cause the ear canal to narrow, leading to significant and sometimes irreparable hearing loss.
The treatment of chronic otitis externa is focused on resolving the underlying cause. During flares, corticosteroid ear drops can help ease inflammation and swelling. Antibiotic ear drops may also be used to prevent bacterial infection.
Other possible complications of otitis externa include:
Abscesses: These painful, pus-filled pockets can form in the ear canal as the infection spreads into hair follicles. Severe cases may require antibiotics and the drainage of pus.
Auditory canal stenosis: Severe or repeated infections can scar the walls of the ear canal, causing the ear canal to narrow. The narrowing (stenosis) may affect hearing.
Eardrum perforation: Infections that spread to the middle ear can cause buildup of pus that weakens the eardrum and causes it to rupture (burst). While the eardrum can usually heal itself in a couple of months, surgery may be needed if it doesn't.
Cellulitis: This severe infection occurs when damaged tissues in the ear canal allow bacteria to gain easy access to deeper tissues. Cellulitis can cause pain, fever, and chills and require a seven-day course of antibiotics to clear.
Necrotizing otitis externa: This is a rare but potentially life-threatening spread of the infection from the ear canal to the base of the skull. The treatment involves intravenous antibiotics (delivered to a vein) and possibly surgery.
While uncomplicated cases of otitis externa can be treated by most healthcare providers, those that are resistant to treatment or cause severe symptoms should be seen by an ENT specialist.
Otolaryngologists are typically at the forefront of the latest treatment approaches and are generally better equipped to perform delicate ear procedures like ear cleanings and otowick placement.
To receive certification from the American Board of Otolaryngology (ABO), applicants must complete medical school and an average of five to seven years of postgraduate surgical training.
It is important to see an otolaryngologist if you experience:
As surgical specialists, otolaryngologists are qualified to perform ear surgeries.
Related: 5 Ways to Prevent Swimmer's Ear
SummaryOtitis externa, also known as swimmer's ear, is an infection of the ear canal, most often by bacteria and less commonly by fungi. It can be caused by getting polluted water in your ear while swimming or putting unclean objects in your ear. Children are affected more than adults. Ear pain, itching, drainage, and hearing loss are possible side effects.
The treatment of otitis externa primarily involves prescription ear drops. These include drying, acidifying, antibiotic, antifungal, and steroid ear drops used either alone or in combination. Oral painkillers (very rarely), ear cleaning, and ear wicks may also be included in the treatment plan.
Chronic otitis externa is a persistent condition more often caused by allergies, autoimmune disorders, and skin disease. It is characterized by itching and hearing loss, often in both ears. The treatment is mainly focused on resolving the underlying condition, but steroid and antibiotic ear drops may be used to relieve inflammation and prevent infection.
Read Next: Types of Ear Infection: How to Tell Them Difference
Hearing Loss And Tinnitus Are Lesser-Known Symptoms Of COVID-19
Hearing Loss From COVID-19 Can Occur Right AwayContracting any virus, including the coronavirus that causes COVID-19, can put you at risk for hearing loss, Hildrew says. This is because once a virus enters the body it starts replicating, and it can do so inside of certain nerves. One of those is the cochlear nerve that runs from your brainstem to your inner ear.
Inflammation from the virus can harm the nerve directly or, because the nerve rests inside a small, bony tunnel, swelling around the nerve can cause damage, he explains.
Hearing loss from COVID-19 can include mild hearing problems where soft sounds are hard to discern; moderate issues where normal speech volume is imperceptible; and severe or profound hearing loss where speech and sounds are inaudible, according to the Centers for Disease Control and Prevention (CDC).
Is It Possible to Cure Hearing Loss From COVID-19?The good news is virus-associated hearing loss during an initial bout of COVID-19 has a high rate of full recovery, Hildrew says. "If you find an ear, nose, and throat doctor quickly — ideally within two days but definitely within a month — there's more than a 60 percent chance all or most of the hearing can come back," he says.
Your doctor will likely perform an examination looking for possible explanations beyond the virus, including ear wax buildup, bacterial infections, or another medical condition. Your physician may also refer you to an audiologist who diagnoses hearing loss with hearing tests including one where sounds and words are spoken at various levels through earphones.
Viral hearing loss is typically treated with steroids to reduce the swelling. These drugs may be given orally or injected into the ear.
An analysis of several studies, published in April 2023 in the European Archives of Oto-Rhino-Laryngology. Found a combination therapy involving oral and injected medicines together may work better than either drug alone.
Hearing Loss Is Also a Possible Symptom of Long COVIDSudden hearing loss can occur in the months and years after someone has recovered from the so-called acute phase of COVID-19, says Zahra Jafari, PhD, a neuroscience researcher at the University of Lethbridge in Alberta, Canada. This makes hearing loss a symptom of long COVID, a condition involving various symptoms lasting three or more months after the initial phase. Figures from the CDC from 2022 showed that 7.5 percent of adults in the United Statse have long COVID.
According to a meta-analysis co-authored by Dr. Jafari and published in April 2021 in Cambridge University Press, some 3 percent of people who had COVID-19 experience hearing loss sometime after having the disease. Most of the research the group analyzed was based on self-reports rather than objective measurements, so more research is needed, the authors wrote. Still, these types of analyses "are the best level of evidence in clinical practice," Jafari says.
A recent study looked at 58 people who have long COVID and reported hearing impairment. In this research, published online in Infection and Drug Resistance in March 2023, the majority were found to have reduced hearing results in subsequent tests. And almost 20 percent lacked a common reflex called the stapes reflex that happens in the middle ear in response to loud sounds.
In many cases, COVID-19 likely speeds up the timetable for hearing problems a person was already developing, Hildrew says.
People may have had mild hearing issues they'd been trying to ignore but that became more obvious during the early phase of the pandemic: Struggling to hear others talking through masks, for instance, made some individuals realize how much they'd come to rely on watching lips move, Hildew says. This may have pushed some people to complain of hearing loss and get tested and treated when they might otherwise have delayed.
COVID-19 Hearing Loss Can Become PermanentHearing loss that is not treated immediately with steroids or does not respond to this treatment is likely permanent, Hildrew says.
In this case, doctors generally recommend a hearing aid if the loss is bothersome. Hearing aids today are smaller and less visible than models were in the past and many have controls accessible through a smartphone to better reduce ambient sound, Hildrew notes.
In addition to hearing aids, the CDC advises people with hearing loss to take advantage of technology like closed captioning for televisions and flashing or vibrating clocks, alarms, or telephones.
Tinnitus Is Another Symptom of Long COVIDSome call tinnitus ringing in the ears, but that doesn't do justice to the condition, Hildrew says. Tinnitus is a constant sound in one or both ears that can resemble buzzing, yelling, a roaring engine, a loud wind, or other disruptive sounds, and can debilitate some people.
Jafari's Cambridge University Press study found tinnitus after COVID-19 is even more likely to occur than hearing loss, affecting 4.5 percent of patients.
Although the causes of tinnitus are unclear, it is likely related to hearing loss. "If we have hearing loss, the brain over activates the [nerve] pathway and by trying to help us hear better creates the setup for this ringing," Hildrew says. Having minor hearing loss from or in addition to COVID-19 causes the brain to ramp up this effort, he believes.
One New Jersey woman developed a number of long COVID symptoms, including tinnitus, as well as fatigue, mental confusion, and a loss of smell. The tinnitus — a constant, high-pitched tone that sounds like someone is shrieking into one of her ears 24/7 — is the most life-altering complication, she says.
How Tinnitus From Long COVID Is Diagnosed and TreatedTinnitus is generally diagnosed by a doctor based on symptoms, but physicians will likely also perform a hearing test and physical exam.
There is no cure for tinnitus. Instead, you're encouraged to find ways to distract your brain. At night — when tinnitus is most bothersome, since a quiet background causes aural sensations to intensify — that might involve turning on a TV or fan or using a white noise machine set to thunderstorms or another sound.
Those who are bothered by tinnitus during the day may benefit from a hearing aid. "With many brands there's a setting you can activate that plays modulating frequencies in the background" for distraction, Hildrew says.
Some people find cognitive behavioral therapy (CBT) helpful. It can't make the sounds go away, but it can help you be a little less bothered by them, Hildrew says.
Does the COVID-19 Vaccine Cause Tinnitus?Online chat groups are filled with people who say their tinnitus started soon after they got a COVID-19 vaccine. More than 12,000 cases were self-reported on the U.S. Government's Vaccine Adverse Event Reporting System (VAERS) as of September 2021, according to a review in the Annals of Medicine and Surgery in March 2022.
The CDC has not formally named tinnitus as a vaccine side effect.
But some other groups have, including a committee of the European Medicines Agency, which determined this was a potential side effect of the Johnson & Johnson vaccine back in 2021. Published case reports that year also linked tinnitus to the mRNA vaccines from Moderna and Pfizer.
A study of 78 million health records across the United States found tinnitus did appear after a COVID-19 vaccine — generally the first shot in the series — but in very few people, scientists reported in The Laryngoscope in September 2022. Just 0.038 percent of vaccine recipients went on to experience tinnitus. And when the researchers compared this rate with other vaccines, they found flu and pneumonia vaccines were responsible for higher rates of subsequent tinnitus.
Still, because so many people have received a COVID-19 vaccine, even a tiny percentage can translate into a lot of people.
How COVID Vaccine–Induced Tinnitus Is TreatedIn some cases, tinnitus that appears after COVID-19 vaccination gets better on its own, Hildrew says.
If it doesn't, treatment is the same as for the illness brought on by the virus itself: distraction via external sounds or a hearing aid.
The most important thing if you suspect hearing issues related to COVID-19 or the vaccine is to contact your medical professional right away.
"Referral for otologic and audiologic services is necessary to determine the type and severity of the auditory disorder, which may help treat, mitigate, or cope with these ear-related issues," Jafari says.

Comments
Post a Comment